Posted by Janine Griffiths
How the assisted dying vote affects end of life care

Something significant happened in June 2025. After years of debate, the House of Commons passed a bill that could change the landscape of end-of-life care in the UK. With a vote of 314 to 291, MPs supported legislation that would allow assisted dying for people with a terminal illness, under strict safeguards.
Now, the Bill moves to the House of Lords, where it will face further scrutiny and discussion. But for many people - particularly those thinking ahead about later life - the question is already here: what does this decision really mean?
The assisted dying vote has opened up a national conversation about choice, dignity and the kind of care we want in our final months. It’s not just a political moment. It’s a deeply personal one, especially for those who are navigating decisions about palliative care, planning for the future, or supporting loved ones through the most vulnerable times of life.
What the vote involved and what it actually means
When something as big as this happens, it's easy to hear the headlines without quite knowing what they mean for you. So let’s break it down.
The assisted dying vote took place in the House of Commons on June 20, 2025. The official name for the Assisted Dying Bill is the Terminally Ill Adults (End of Life) Bill. The Bill will need to pass through the House of Lords before becoming law. It means Parliament is now one step closer to legalising assisted dying for adults in England and Wales who are living with a terminal illness.
The proposal comes with very specific conditions. To qualify, a person must have been given less than six months to live. Two independent doctors would need to agree on the diagnosis. There would also be a formal review by a specialist panel before anything could go ahead. These safeguards are designed to protect the vulnerable while giving choice to those facing unbearable suffering.
Nothing is final yet, but this is the furthest such legislation has ever gone in the UK. And for many people, especially those thinking carefully about their future, the outcome of the assisted dying vote is now impossible to ignore.
What it means for people facing a terminal diagnosis
This part of the conversation is, understandably, the most emotional. When someone receives a terminal diagnosis, life can begin to feel like it's no longer theirs to shape. Options shrink. Time becomes both precious and uncertain. That’s why this moment matters so much.
The assisted dying vote represents a turning point. For the first time in the UK, the idea of having a legal, medical option to end your life with dignity is no longer just a debate. It is now a possibility being taken seriously by lawmakers. For those living with a terminal illness, that alone can change the emotional landscape.
It's not about encouraging anyone to make one decision or another. It’s about knowing there might be a choice. That you don’t have to be trapped in pain or fear, and that there could be a supported, compassionate route if suffering becomes too much.
For many, simply having that option brings a sense of peace. Even if it’s never chosen, it offers a quiet reassurance that autonomy hasn't completely slipped away. This reflects a growing public belief that people nearing the end of life deserve the right to decide how they leave it, just as much as how they live it. The assisted dying vote is not just a legal step forward - it is a deeply human one.
The controversy around assisted dying
However, not everyone is in favour of assisted dying.
Some of the opposition around the assisted dying Bill is due to religious beliefs or fears that in some cases, it could actually take away autonomy.
It is no surprise that religious organisations have spoken out against the Bill over fears MPs are “playing God” by allowing terminally ill people to end their life. Just recently, it was reported that Chris Coghlan, the Liberal Democrat MP for Dorking and Horley in Surrey was denied communion by his local Catholic priest after backing the Terminally Ill Adults Bill.
Others have expressed concern that in the future, the proposed Bill could be modified and amended in a way that weakens the current safeguards and results in people dying prematurely.
For instance, the British Medical Association has outlined a range of arguments both for and against the assisted dying vote. Concerns raised include the risk of coercion, fears that the law could change how society views older people and worries that doctors might feel pressured to take part in procedures they do not support. They also expressed concern that over time, the eligibility criteria for assisted dying could be widened and that the focus should be on ensuring patients have access to universal high-quality care.
Safeguards and professional readiness
The concerns around the assisted dying vote are understandable. The whole purpose is to ensure people are afforded dignity, choice and comfort during end-of-life care and so it makes it all the more essential that the safeguards put in place are effective in preventing any unintended and potentially fatal consequences. In addition to the proposed safeguards of requiring 2 doctors and a panel to review assisted dying requests, the BMA has called for extra layers of protection, including more in-person assessments to help ensure that no one is being pushed or influenced against their will. These include making sure that doctors are not pressured to prematurely bring a patient's life to an end, and ensuring patients get access to high quality, holistic palliative care, regardless of whether that care takes place at home or in a residential facility.
One thing is clear. If the law passes, systems will need to be in place and this will require comprehensive training for staff, clear protocols, expert review panels and independent advocates who can support people through the process. It’s not just about changing the law. It’s about making sure the people behind it are ready to meet this moment with thoughtfulness and humanity.
Pressure on palliative and hospice care
The assisted dying vote has not only opened up questions about choice but also cast a spotlight on the state of end-of-life care more broadly. For many, the decision to back the Bill has been as much about what is missing in current care systems as it is about what should be added.
Palliative and hospice services across the UK are under strain. Most hospice care is funded largely by charitable donations, with only a small percentage coming from the government. That imbalance puts pressure on providers and can leave families feeling uncertain about what kind of support is available when they need it most. In light of the assisted dying vote, this concern has become more urgent. Some organisations have warned that unless palliative care is properly funded, people may feel that assisted dying is their only real option.
The NHS has also raised financial questions. Setting up a safe, regulated system for assisted dying could cost millions each year, and that investment would need to sit alongside renewed commitments to hospice and end-of-life care.
Ultimately, the vote has done more than introduce a new choice. It has asked a bigger question: are we doing enough to support people through the final stage of life, no matter which path they take?
Broader implications for families
When you're planning for later life, clarity can make all the difference. Most families already face a long list of decisions when it comes to care from choosing between home care or residential care, to navigating costs, eligibility, and support. Now, following the assisted dying vote, there’s an entirely new layer to consider.
The introduction of a legal route to assisted dying, if it becomes law, adds complexity to conversations that are already emotional and often overwhelming. Families will need to understand not only palliative care options, but also how this new choice might be supported, discussed, or approached by care providers. It’s not always easy to talk about, but it will become increasingly important to do so.
For those funding their own care his raises practical questions. Will providers be transparent about their stance? Will families be able to find the right fit for their personal values and beliefs? As people look for control and reassurance in how they are cared for, the assisted dying vote brings a quiet reminder that it’s not just about care - it’s about confidence in your choices and the people who will stand by them.
What comes next and why it matters
So, what now? With the assisted dying vote passed in the House of Commons, attention turns to the next stage of the journey and it's an important one.
The passage of the Bill through the house of Lords will take time, and rightly so. The subject is complex, emotional, and touches on deeply personal beliefs. If the Bill clears this stage, it could receive royal assent by the end of 2025, making assisted dying legal in England and Wales. Implementation, however, would not be immediate. It could take up to four years to put the right safeguards and systems in place.
For anyone thinking about their later life, this isn’t just politics in motion. It's about understanding how change might shape your choices, care and peace of mind. The assisted dying vote may have started in Parliament, but its impact reaches much closer to home.
A changing landscape of care and choice
As the conversation continues to unfold, one thing is clear: something has shifted. Whether or not the Bill becomes law, the assisted dying vote has already marked a turning point in how we prepare for and experience the final chapter of life.
It has stirred emotions, raised questions, and reminded us all of the importance of dignity and choice. But just as importantly, it has highlighted the urgent need to strengthen palliative and hospice care, so that no one ever feels they are choosing assisted dying because good care is out of reach.
This moment invites us to think more openly about what we want from our later years and how we can ensure those wishes are respected. It's not only about endings. It's about being seen, heard and supported every step of the way. The future of end-of-life care may be changing, but humanity should always remain at its heart.
Looking for end of life care?
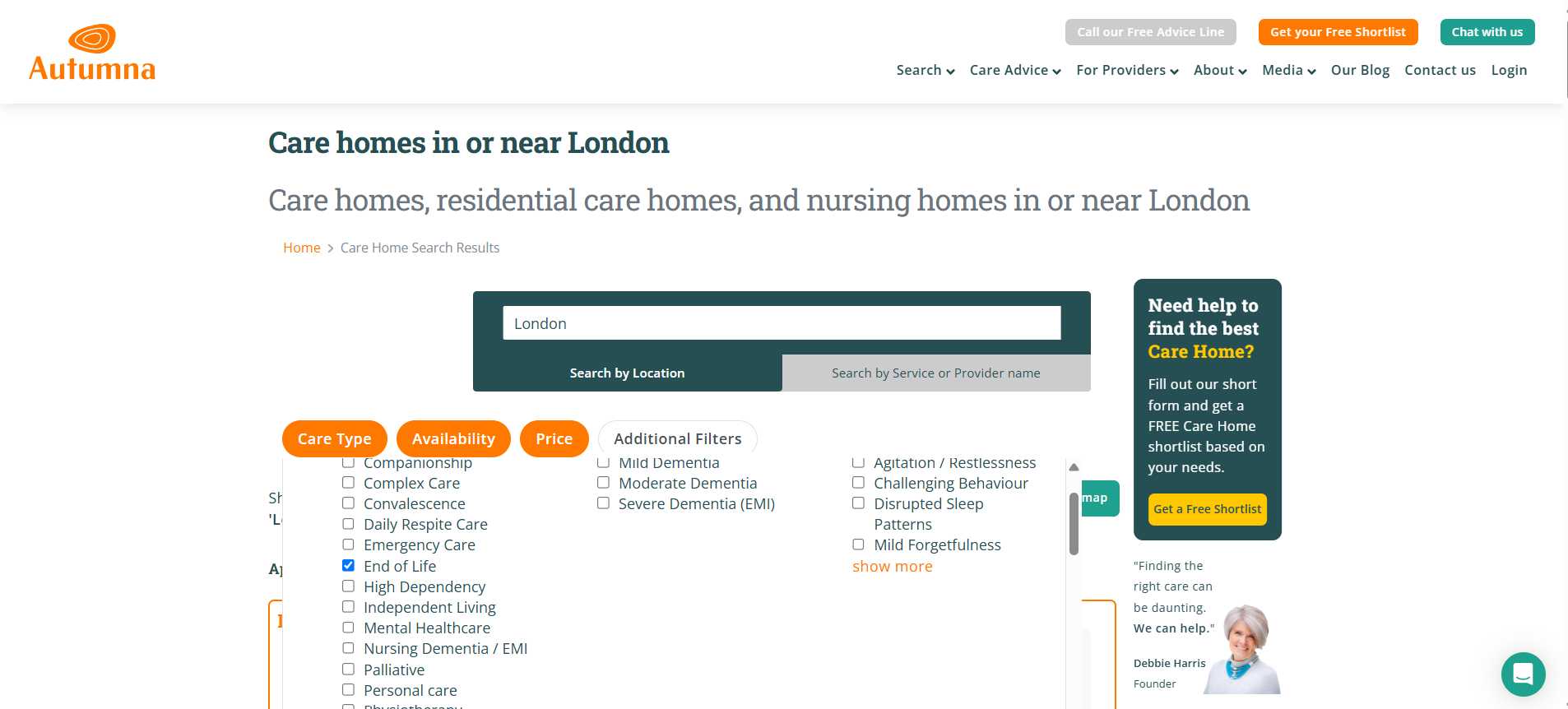
Finding end-of-life care can feel overwhelming, but Autumna is here to make it simpler. Start by visiting our online directory and entering the location you want to search in. Then, open the ‘Additional Filters’ section, choose ‘Care Given’, and select ‘End of Life’. Click ‘Search Again’ to view care homes in your chosen area that provide this type of support.
Prefer a helping hand? You can fill out a short questionnaire and let our expert team do the searching for you. Or, if you’d rather speak to someone directly, call our friendly Advice Line on 01892 335 330. We're here to help every step of the way.
Receive a Free Care Provider Shortlist!
Let our expert team of advisers get your search off to a great start.
Tell us a little about your needs and we'll send you a bespoke shortlist of care providers! Click the button below to begin, it takes just a few minutes.
Other articles to read
From the blog

Older Persons Care Advice
How to talk to your parents about care options
October 2nd, 2025
Learn how to talk to your parents about care options with compassion. Explore choices together and plan for the future with dignity and respect.

Older Persons Care Advice
Guide to empowering and promoting independence in older age
September 30th, 2025
Read our practical guidance for families on empowering and promoting independence in older age, helping loved ones stay confident and in control.

Older Persons Care Advice
Ultimate guide to jointly owned property and care home fees
September 26th, 2025
Understand jointly owned property and care home fees, how assessments work, and steps to protect your finances and plan ahead with confidence.
Frequently Asked Questions
If the Bill becomes law, healthcare professionals who object to assisted dying on moral or religious grounds would have the legal right to opt out. However, systems would be put in place to ensure the individual seeking assisted dying is referred to a willing and qualified practitioner. The law would aim to protect both patient rights and professional conscience.
No, care homes would not be forced to offer assisted dying. Providers would likely be allowed to state their position clearly, and residents or families would need to choose a setting that aligns with their values and preferences. This is why transparency will be critical going forward.
Under the current draft of the Bill, individuals must have the mental capacity to make the decision themselves and must be diagnosed with a terminal illness with a prognosis of six months or less. This would exclude most people with advanced dementia, although the criteria could be revisited or revised in future debates.
Not directly, but the debate has highlighted the need for improvements in palliative and hospice services. Some argue that legalising assisted dying must go hand-in-hand with better access to high-quality care, so no one feels pressured to choose assisted dying due to lack of support.
Even if the Bill receives royal assent by the end of 2025, implementation would not be immediate. Experts estimate it could take up to four years to establish the necessary training, infrastructure, protocols and safeguards before assisted dying becomes available in practice.






